In hemofiltration, the removal of plasma water under pressure essentially “drags” solutes with it, leading to their removal, a process referred to as convection. This mechanism allows for superior middle molecule clearance compared to dialysis, which has led many clinicians to propose hemofiltration as the preferred method of renal replacement therapy (RRT) in cases of septic acute kidney injury (AKI).
How Hemofiltration Works
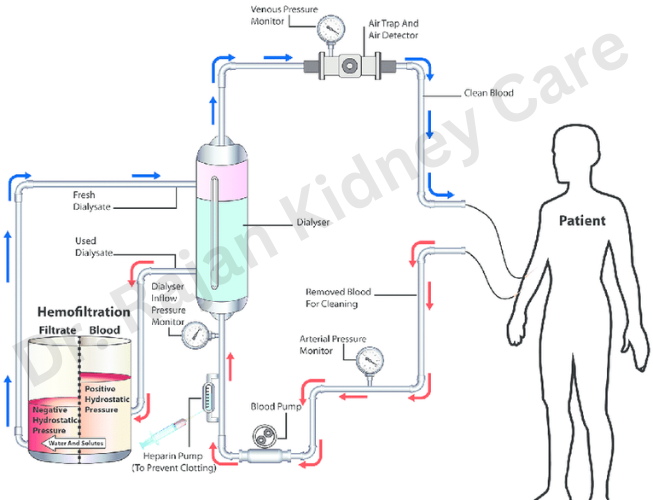
Blood is obtained from the patient through a catheter or access point, usually inserted into a large vein.
The blood is then passed through a hemofilter, which contains a semi-permeable membrane. This filter allows for the removal of small and middle-sized molecules, including waste products and excess fluids, while retaining larger molecules such as blood cells and proteins.
To maintain fluid balance and replace lost fluids, a replacement fluid (often referred to as ultrafiltrate) is infused into the blood after it has passed through the filter. This fluid helps ensure that the blood’s composition remains stable.
The filtered blood, now free of waste products and excess fluids, is returned to the patient’s body.
Types of Hemofiltration
This method is often used in critically ill patients, where blood is continuously filtered and replacement fluids are continuously infused.
It Combines hemofiltration with dialysis to remove a wider range of waste products, utilizing both convection (hemofiltration) and diffusion (hemodialysis).
It is often used to remove excess fluid from the body in addition to waste products.
